You may have heard about BiTE therapy, but what is it and how does it work? Let’s explore this exciting new immunotherapy option for those facing cancer.
Bispecific T-cell engager (BiTE) therapy is a type of immunotherapy that is designed to trigger a patient’s own immune system. Cancers can hide from the immune system. BiTE therapy directs certain immune cells, called T-cells, to attack and kill cancer cells.
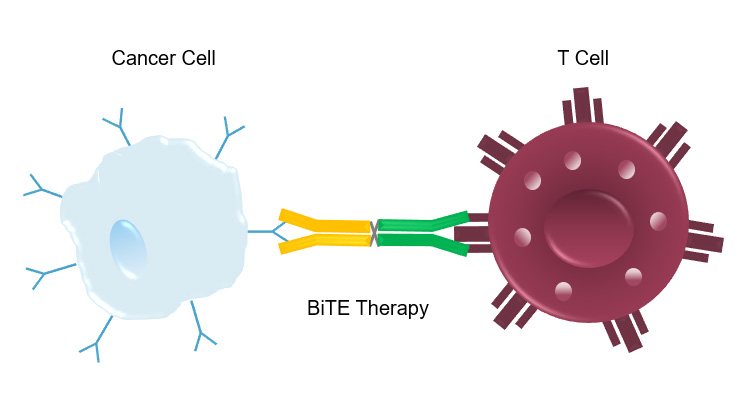
T-cells typically need help to identify cancer cells, a task that is accomplished by other immune cells in the body. Cancer cells often learn to dampen or shut down the immune system such that it becomes hard for T-cells to find them. BiTE therapy overcomes this challenge by serving as a connector between the T-cell with the cancer cell. Let’s think of BiTE as a lasso. One end hooks on to a protein on the T-cell (called CD3) and the other end attaches to an antigen on the cancer cell and reins both of them in next to each other. This allows the T-cells to “lasso” the antigen-marked cancer cell and destroy it. While the name “bispecific T-cell engager” may be a mouthful – it describes exactly what the therapy does – engages T-cells to seek and destroy cancer cells.
This therapy engages a patient’s own body to fight off cancer. Depending on the type of cancer being treated, it could be started after multiple rounds of standard chemotherapy or earlier in the course of disease. Since BiTE therapy harnesses the body’s immune system, it can be associated with unique side effects that are different than typical chemotherapy, such as an inflammatory state called “cytokine release syndrome” and certain infections that are more common in immunocompromised patients. Your medical team will determine if this is a useful treatment for you.
Currently, this therapy is available to patients with certain cancers as an FDA-Approved medication and through clinical trial options. For more information on clinical trial options, please visit the Sarah Cannon Research Institute website.